Despite recording and storing every call, most organizations analyze only about 2% of these conversations. There is a steep opportunity cost in the form of lost actionable insights that they could use to increase compliance, reduce hold times, identify errors in patient data processing, and uncover missed sales opportunities.
The real question is, what are healthcare companies missing by ignoring 98% of their customer conversations? The answer is a lot. By failing to analyze their interactions thoroughly, organizations miss opportunities to optimize operational efficiency, leverage revenue prospects, improve service quality and loyalty, and prevent compliance risks and potential fines.
To understand the full impact of this oversight, let's examine the specific challenges faced by healthcare contact centers, how they contribute to poor performance, and how conversation intelligence can turn missed opportunities into contact center wins.
Quantifying Poor Contact Center Performance
Healthcare contact centers face unique challenges that can drive up operational costs and negatively impact the customer service experience. Some of these pain points include:
Complicated topics lead to complex interactions
According to CFI Group, more than 72% of healthcare consumers still pick up the phone first when they need customer service. In an age where consumers have come to expect quick responses and fast issue resolution, long hold times are a critical liability.
Healthcare interactions are complex, yielding lengthy average talk times. Members and patients reach out to care teams for a wide variety of reasons—ranging from simple appointment scheduling to nuanced benefits or billing issues. The breadth and complexity of these calls may require representatives to spend time searching for the correct response, which can translate into extended handling and hold times. Longer talk time translates into agents taking fewer calls, which, in turn, extends hold times for other callers. These factors contribute to dropped calls, lower customer satisfaction scores, and even loss of business.
There are ways to reduce the average handling time (AHT), but without reviewing all your patient and member conversations, it’s impossible to pinpoint effective solutions that could drive improvements at scale.
Compliance risks
Manually entering caller information or failing to capture critical details during a call can lead to mistakes that result in HIPAA or GDPR violations. Agents neglecting to follow scripts or provide critical disclosures carefully can also lead to non-compliance. The result? Hefty fines, reputational damage, potential lawsuits, and loss of customers and revenue.
Contact centers must also spend inordinate time training care teams on regulatory guidelines as they evolve. This is an expensive proposition, tying up key staff who could be working on other, more high-value activities.
The sum of all these issues boils down to this: lack of compliance with internal processes and external regulations can cost a healthcare organization hundreds of thousands of dollars a year.
Operational inefficiency
Many healthcare contact centers rely on manual processes and inefficient, time-consuming, error-prone workflows. Representatives spend excessive time searching for information, entering data, performing after-call work, and toggling between multiple software platforms during interactions. Large team-lead-to-agent ratios make delivering proper individual coaching and resource planning and allocation impossible. With many contact centers employing 1 QA per multiple team leads, it is virtually impossible to manually QA all calls and drive meaningful results.
So, the contact center team can continue to “survive,” barely meeting its growing goals and high customer expectations. Or, they can turn to technology to solve some of their biggest challenges and redefine their contact center as a strategic, cost-optimized revenue driver.
The Solution: Adding Conversation Intelligence
Conversation intelligence solutions with artificial intelligence (AI) and automation can analyze 100% of conversations, identifying key patterns and offering insights to dramatically improve contact center performance.
Here’s how it addresses the issues above:
Call efficiency + caller satisfaction
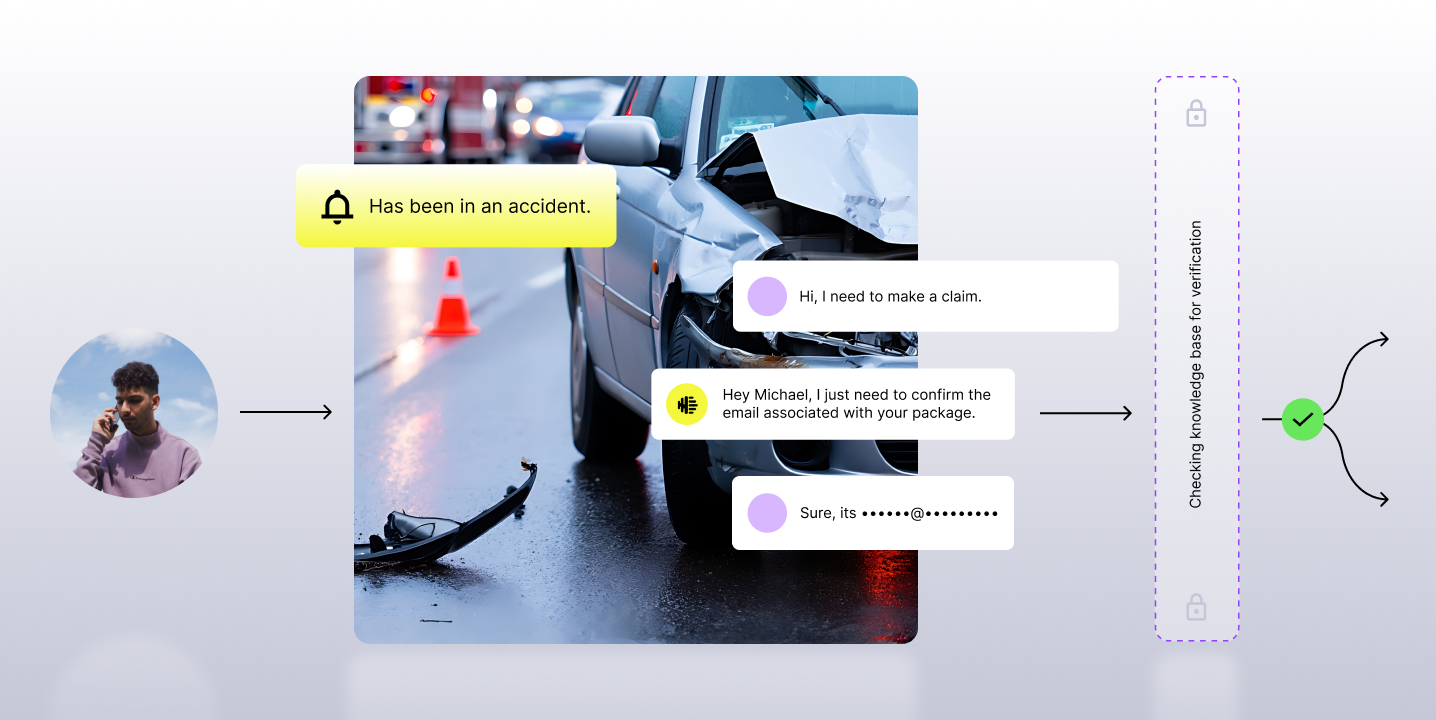
Conversation intelligence offers real-time agent assist scripts, prompts, and recommendations to ensure every representative follows best practices to complete each call as efficiently as possible. To address more complex inquiries, these technologies leverage AI to scan the healthcare organization’s knowledge bases and equip representatives with accurate information at the right time, improving first-call resolution, reducing the need for follow-up or repeat calls, and enhancing efficiency. Conversation intelligence also enables real-time call summaries, reducing representatives' after-call work.
These real-time assistance and post-interaction tools enable your representatives to deliver higher-quality service to more people–improving your contact center's performance and customer experience.
Improving procedural and regulatory compliance
Monitoring 100% of conversations allows healthcare companies to identify compliance risks and offer immediate alerts when something veers off track. This proactive approach ensures contact centers comply with regulations and reduces the risk of costly fines.
Using AI to provide scripts and prompts can help representatives adhere to internal procedures and regulatory requirements, yielding greater efficiency and optimized outcomes. This also enables compliance teams to effectively distribute new requirements to their personnel, reducing overall risk.
Operational efficiency + growth
Conversation intelligence enables contact centers to maximize their current resources and impact. Automating QA for 100% conversation analysis provides visibility into what's working and what’s not, enabling you to optimize processes, coaching, and cost. It also yields greater customer satisfaction and reduced compliance risks.
Additionally, analyzing all of their customer conversations enables healthcare organizations to uncover more unmet needs and pain points. They can use these insights to create new products and services to enhance revenue, address common issues, and improve retention rates.
Sales teams can tailor offerings based on real-time feedback, providing a clear cost-benefit to the organization. Listening closely to customer needs during these conversations also boosts conversion rates and loyalty.
Real-World Impact
MaxorPlus, a pharmacy benefit manager, faced challenges with agent performance and customer experience in its contact centers. By integrating screen recording, as well as Observe.AI’s conversation intelligence and agent coaching, MaxorPlus transformed its contact center operations.
The solution allowed the company to monitor 100% of customer interactions, providing real-time coaching and agent feedback. This significantly reduced errors and increased compliance. The company saw a marked improvement in overall operational performance, reducing average handling time by 7% and increasing customer satisfaction by 2%. The screen recordings gave managers deeper insight into agent behavior, enhancing training efforts and customer outcomes.
This type of transformation isn’t unique. Numerous healthcare providers and payers are reaping the rewards of using AI-driven conversation intelligence to overhaul their contact center operations, with similarly impressive results.
Takeaway
Healthcare organizations already spend the money to collect and store their conversations. So why not leverage this data to drive cost, efficiency, and growth opportunities? Conversation intelligence helps organizations realize the full potential of every interaction by turning them into actionable insights. It’s time to leverage this groundbreaking technology to unlock new possibilities for your customers, contact center operations, and your entire organization.